The legacy of the H1N1 swine flu outbreak will long outlast the appearance of new cases. The tourism industry in Mexico, where the illness first appeared last spring, could be hit hard, as could the economy at large, depending on how the virus behaves in the months to come. Foreign tourism earned Mexico $13.3 billion last year, employs more than 2 million people, and accounts for 8 percent of the economy. Mexican government officials, who initially imposed draconian restrictions on public gatherings and travel, have estimated that the loss of revenue could be as much as $5 billion and might lower the gross domestic product 0.3–0.5 percent. Final figures will not be available until early next year.
Mexico was not the only country to have instituted drastic measures during the outbreak. China imposed strict quarantines on contacts of confirmed cases and restricted air travel from Mexico, and Egypt slaughtered all its pigs. Arguably, some of these interventions were excessive, but is excess in the name of public health a bad thing? That question requires complex cost-benefit assessments. Overly conservative, risk-averse actions can have dire consequences. The loss of revenue exerts an income effect that reflects the correlation between wealth and health. The accumulation of wealth by societies is necessary to build schools, support infrastructure and sanitation, and improve environmental amenities. It is no coincidence that richer societies have lower mortality rates and cleaner environments than poorer ones. Thus, to deprive communities, or individuals, of wealth (particularly in poor countries) is to increase their health risks; the health effects include a rise in stress-related problems such as ulcers, hypertension, heart attacks, depression, and suicide.
It is difficult to measure the relationship between the deprivation of income and mortality, but academic studies suggest that every $5 million to $10 million in lost revenue will induce one additional fatality. (Thus, the conservatively estimated direct and indirect costs of the loss of revenue to Mexico could cause about one thousand deaths there—almost ten times the nation’s death toll from the H1N1 flu.)
The World Health Organization (WHO), an agency of the highly politicized United Nations, did Mexico no favors. Its decisions and pronouncements were far from reassuring. Most flu and public health experts consider WHO to have been overly alarmist and maintain that its decision during the week of April 27 to raise the flu threat to the penultimate level five, “pandemic imminent,” far outpaced the available data. Even worse was its June 11 elevation of the threat to level six: pandemic. A warning system, based solely on how widely a virus has spread, that does not consider the nature of the virus-induced illness is prone to false positives: it would classify as pandemics the frequent but largely inconsequential outbreaks of virus-caused colds and gastroenteritis.
WHO’s flawed decision making illustrates that its officials are either too rigid or too incompetent to make needed adjustments in the warning system. WHO, an organization that is scientifically challenged, selfimportant, and averse to transparency, may be well equipped to perform and report worldwide surveillance, but its policy role should be drastically limited.
The decisions that need to be made in such cases are difficult, encompassing virology, medicine, economics, and ethics. Should nations close borders and restrict domestic and international travel and trade? Should public health officials rush to prepare vast amounts of vaccine?
Closing borders, besides severely disrupting commerce and the creation of wealth as described above, would deny access to many items made abroad that are needed during a pandemic, including masks, gloves, ventilators, and certain pharmaceuticals and their precursors. Still, many national public health officials, especially those in countries that suffered from the 2002–3 SARS outbreak, tend to be overly conservative to avoid any possible accusation of having been too timid. Alarmist declarations from WHO spur them on to further risk-averse actions that are neither necessary nor cost-effective.
The vaccine issue is complex. Even if pharmaceutical plants had begun to formulate and manufacture vaccines immediately, they would have arrived far too late to significantly attenuate the first wave of infections. Such a crash program to manufacture vaccine could possibly blunt subsequent waves, if they occur. Historically, flu pandemics have come in two or three waves, lasting a total of thirteen to twenty-three months. In the devastating 1918–20 Spanish flu epidemic, which killed perhaps 50 million people worldwide, the vast majority of deaths occurred during a second wave that hit several months after the first (possibly following a genetic change in the virus during its sojourn in the Southern Hemisphere during the southern winter).
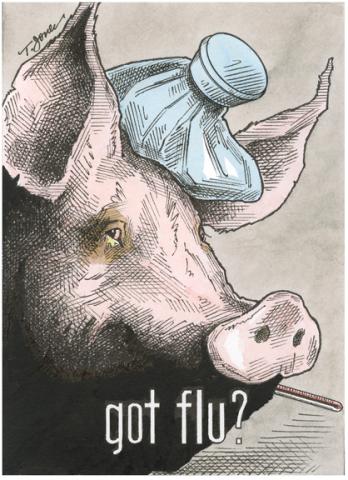
But producing a swine flu vaccine could also occur at the expense of the vaccine against the following winter’s seasonal flu, an annual ailment that kills 30,000–40,000 people every year on average in the United States and ten times that many worldwide—even when a significant fraction of the population is immunized with an effective vaccine. Often the pandemic strains are both qualitatively and quantitatively worse than the seasonal ones, but this pattern apparently has not held for the new H1N1-caused swine flu. If it had, a high proportion of those infected would have required hospitalization for pneumonia, with a correspondingly high death toll. Except in Mexico (for reasons that remain unclear), however, illnesses have generally been mild, hospitalizations few, and mortality low.
Outbreaks of new pathogens require policy makers worldwide to make vexing cost-benefit decisions, but the bureaucrats at the WHO and other United Nations agencies will be of little help. In the long term, we need to rethink the mandates, management, and accountability of this organization. The health of the world’s population is too important to be entrusted to policy makers who are as ambitious as they are unaccountable.