My father was able to recall the “Spanish flu” pandemic during the winter of 1918–19, when classes in his Philadelphia grade school were canceled for weeks, shops were closed, and open horse-drawn wagons filled with corpses rumbled through the cobblestoned streets. Fortunately, as an eight-year-old, he could hardly have grasped the big picture—in October 1918, 195,000 Americans died (11,000 in Philadelphia alone). At one point the deaths came so fast that coffins, which were in short supply, were being stolen. Finally, on March 26, 1919, the government announced that the epidemic had killed 583,135 Americans. About half of those struck down were young and healthy.
JET-AGE PANDEMIC
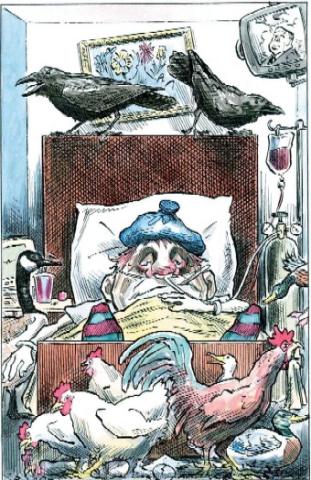
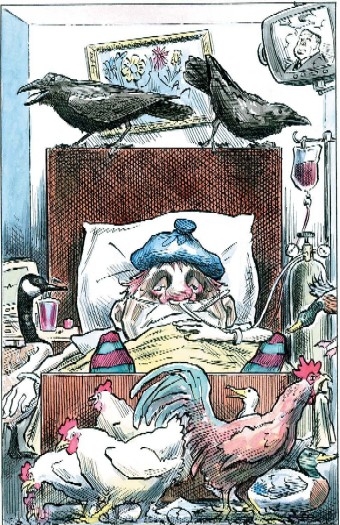
During the past several years, an especially virulent strain of avian flu, designated H5N1, has ravaged flocks of domesticated poultry in Asia and spread to migratory birds and (rarely) to humans and other mammals. It has been detected in much of Europe, Asia, Africa, and the Middle East, and it continues to spread with each seasonal migration of wild birds. Since 2003, there have been about 200 cases of H5N1 infection in humans and more than 100 deaths (a shockingly high mortality rate for an infectious disease).
Public health experts and virologists are concerned about the potential of this strain because it already possesses two of the three characteristics needed to cause a pandemic: It can jump from birds to humans and can produce a severe and often fatal illness. If additional genetic evolution makes H5N1 highly transmissible among humans—the third characteristic of a pandemic strain—a devastating worldwide outbreak could become a reality. The ease and frequency of worldwide travel could give rise to the first true jet-age flu pandemic.
| To treat 150 million people with Tamiflu for 200 days, we would need 30 billion doses. Each pill retails for about $8, so the total retail cost would be approximately $240 billion. That’s not chicken feed. |
It is not possible to predict the timing of that last evolutionary step because the genetic changes that will give rise to it are wholly random molecular events—mutations occur each time the virus replicates, so the more H5N1 viruses that are produced the more likely it is that the event will occur. And as avian flu spreads and more birds are infected, trillions more virus particles come into existence every day. Flu can also evolve when both human and animal strains of flu infect a person or animal simultaneously, offering an opportunity for swapping genes. That process is also favored by the presence of more viral particles in more locations around the world.
Some background is necessary to understand the threat—and the possible public health, economic, and political consequences—of a flu pandemic. The exterior of the flu virus consists of a lipid envelope from which project two surface proteins, hemagglutinin (H) and neuraminidase (N). The virus constantly mutates, which may cause significant alterations in either or both of these, enabling the virus to elude detection and neutralization by the human immune system. A minor change is called genetic drift; a major one, genetic shift. Genetic drift is the reason that flu vaccines need to be updated from year to year; an example of genetic shift was the change in subtype from H1N1 to H2N2 that gave rise to the 1957 pandemic. This new variant was sufficiently distinct that people had little immunity to it: The rate of infection with symptomatic flu that year exceeded 50 percent in urban populations, and 70,000 died from it in the United States alone.
Ordinary seasonal flu—marked by high fever, muscle aches, malaise, cough, and sore throat—is a bad disease that kills 30,000–40,000 annually in the United States, but the pandemic strains are often both qualitatively and quantitatively worse. They infect the lower as well as the upper respiratory tract—that is, deep down in the smaller airways—and often elicit hemorrhage and “cytokine storm,” an outpouring of hormone-like chemicals that causes huge amounts of fluid to accumulate in the lungs. In this way, these pandemic strains of flu may kill within 24 to 48 hours of the onset of symptoms. Seasonal flu most often kills not directly but via secondary bacterial infections that follow the initial viral infection.
| If genetic evolution makes the H5N1 virus highly transmissible among humans, a devastating worldwide outbreak could become a reality. The ease and frequency of worldwide travel could give rise to the first true jet-age flu pandemic. |
DRESS REHEARSAL
The December 2005 outbreak of H5N1 avian flu in Turkey—birds infected in more than 20 localities, about two dozen confirmed human cases, and several deaths within about a month—might be thought of as a kind of dress rehearsal for what an actual pandemic would look like in its earliest stages if the virus were to mutate and become transmissible from person to person. If the Turkish outbreak had been the beginning of a pandemic, we would have expected to see illness spreading through families and among both health-care workers and patients in hospitals where the victims were treated. The rapidity of such a spread would depend on the infectiousness of the pandemic strain, another variable that we cannot predict. Before long, infected persons (perhaps even carriers who aren’t ill) would introduce it to Ankara, Istanbul, Tbilisi, Damascus, Baghdad, and then beyond.
With no effective vaccine available, little could be done to attenuate significantly the first wave of infections. If we’re able to rush the pandemic strain into a crash program to manufacture vaccine, we could possibly blunt the second wave, however.
Much has been made of whether we can significantly ramp up production of two antiflu drugs, Tamiflu and Relenza; but they are far from a panacea under the best of circumstances, and their usefulness is becoming more problematic as we learn more about their interactions with H5N1. Unlike vaccines, which confer long-term immunity after one or two doses, drugs need to be taken for long periods. The only drug that has been shown to prevent the flu is Tamiflu, the usual prophylactic dose of which is one tablet a day, the effect lasting only as long as one takes the drug. (The other major antiflu medicine, Relenza, has been shown to be effective only to treat, not prevent, flu.)
| In places where the pandemic strain will likely originate (China, Vietnam, Indonesia), animal husbandry practices, unsanitary conditions, poverty, and grossly inadequate public health infrastructures make it highly unlikely that a pandemic can be prevented or contained at the source. |
Historically, flu pandemics have come in two or three waves, lasting a total of 13–23 months. In other words, the need to take Tamiflu—by first responders, health-care workers, and ordinary citizens—could go on for months or even years. According to various models, in the absence of sufficient amounts of an effective vaccine—which is not yet within reach—to blunt the first wave of the pandemic in the United States, we would need to treat perhaps half our population with Tamiflu. Do the math: To treat 150 million people for 200 days, we would need 30 billion doses. Each pill retails for about $8, so the total retail cost would be approximately $240 billion. That’s not chicken feed.
And that seems to be the best-case scenario because there are now credible reports that H5N1 is less sensitive to Tamiflu than other strains of flu and that some mutants of H5N1 are resistant to Tamiflu.
STRATEGIZING
Despite the fact that the possibility of a flu pandemic has been taken seriously by scientists, governments, and businesses around the world, there has been some skepticism—mostly from nonscientists—about the imminence and possible impact of an H5N1 pandemic. Laura Kelley, an associate of the National Intelligence Council (writing in her private capacity), wrote, “Remarkable though it may seem, all of this spending and activity is based on the deaths of fewer than seventy-five people, caused by a viral strain that has little or no person-to-person transmissibility.” That is rather like saying that, because it hasn’t caused any damage yet, we don’t need to worry about a Category 5 hurricane on a track to hit New Orleans. Journalist Tom Bethell ascribes the attention paid to avian flu to “a shared interest” between public health agencies and the press: “One wants a bigger slice of the budget and the other wants greater circulation.” Bethell may be right about the existence of hidden agendas. But the threat remains real.
What should be our strategy toward H5N1? In theory, it is possible to contain a flu pandemic in its early stages by performing “ring prophy-laxis”—using antiflu drugs and quarantine aggressively to circumscribe and isolate relatively small outbreaks of a human-to-human transmissible strain of H5N1. According to Johns Hopkins University virologist Donald S. Burke, “models show that it may be possible to identify a human outbreak at the earliest stage, while there are fewer than 100 cases, and deploy international resources—such as a [World Health Organization] stockpile of antiviral drugs—to rapidly quench it. This ‘tipping point’ strategy is highly cost-effective.”
| China’s prodigious effort to vaccinate 14 billion chickens annually has been chaotic, compromised by the appearance of significant amounts of counterfeit vaccines and by the absence of protective gear for vaccination teams. |
However, a strategy can be cost-effective only if it’s actually feasible. Although ring prophylaxis might work in Minneapolis, Toronto, or Zurich, in the parts of the world where flu pandemics begin, the probability of success approaches zero. In places such as Vietnam, Indonesia, and China— where the pandemic strain will likely originate—intensive animal husbandry procedures that place billions of poultry and swine in close proximity to humans, combined with unsanitary conditions, poverty, and grossly inadequate public health infrastructure of all kinds, make it highly unlikely that a pandemic can be prevented or contained at the source.
China’s prodigious effort to vaccinate 14 billion chickens annually has been chaotic, compromised by the appearance of significant amounts of counterfeit vaccines and by the absence of protective gear for vaccination teams—who might actually spread disease by carrying fecal material on their shoes from one farm to another. In Turkey, although local officials in the region where the bird flu first was detected warned the federal government on December 16 of a surge in bird deaths, it took another 12 days for an investigation to begin. And when in early January a 14-year-old boy became Turkey’s first avian flu mortality (followed soon by two siblings), a government spokesman criticized doctors for mentioning the disease because they were “damaging Turkey’s reputation.” These responses ominously resemble the passivity and denial by the Chinese government during the SARS outbreak of 2003.
We need good surveillance of H5N1 in Europe, Asia, and Africa to obtain the earliest possible warning that a strain of H5N1 flu transmissible from human to human has been detected, so that nations around the world can rapidly initiate a variety of public health measures—not the least of which would be to begin an emergency program to produce large amounts of vaccine against that strain.
The U.N.’s World Health Organization is probably best equipped to perform surveillance, but its role must be limited. Dr. David Nabarro, the U.N. coordinator on avian and human influenza, who has wide experience as a public health bureaucrat but none in the highly specialized field of influenza, is busily raising money from countries around the world to finance efforts to combat the disease. However, we cannot ignore the dismal record of the scientifically challenged, politically correct, unaccountable United Nations and the reality that any component of it is inherently incapable of keeping politics out of scientific and medical decisions.
The best hope for coping with a pandemic is that it won’t occur within a year or two and that vaccine development will advance significantly before it strikes. The limitations of current vaccine production methods slow our response to the constantly appearing new variants of seasonal flu virus. Decisions about the viral strains to be included in every flu season’s vaccine must be made during the previous winter, and the viruses are then grown in scores of millions of chicken eggs. In the face of a pandemic, this lag could be catastrophic. Moreover, note that in the face of a pandemic, virtually the entire world’s flu vaccine capacity will turn to production of vaccine against the H5N1 pandemic variant, leaving populations vulnerable to the seasonal strains. (These seasonal influenza strains kill 30,000–40,000 annually in the United States, even when a significant fraction of the population is immunized with an effective vaccine.)
| Initial Turkish government responses to the H5N1 outbreak ominously resemble the passivity and denial by the Chinese government during the SARS outbreak of 2003. |
A few companies are taking innovative approaches to vaccine development, potentially the most important of which is the use of gene-splicing techniques to make so-called subunit flu vaccines. Used for two decades to produce Hepatitis B vaccine, this approach involves moving a single gene (or a small number of genes) from the virus into bacteria or yeast; then, grown at large scale, these organisms are the source of the viral gene product that, after being isolated and purified, is used as the vaccine. The culmination of this approach would be a vaccine that elicits an immune response to the proteins of flu virus that are highly conserved from strain to strain.
However, flawed public policy inhibits research and development on vaccines. The major purchaser of most vaccines in the United States, the Centers for Disease Control and Prevention (CDC), exacts huge discounts from manufacturers, and arbitrary and excessive regulation by the Food and Drug Administration also blocks progress. As a result, innovation has suffered and vaccine producers have abandoned the field in droves, leaving only four major U.S. manufacturers and a few dozen products. For example, until about a year ago, there were only two producers of injectable flu vaccine for the U.S. market.
Government deficiencies have caused many of these problems, and federal initiatives will need to be part of the solution. Grant-giving agencies should increase funding for basic research on subunit vaccines, especially those that are “cross-subtype-specific” (effective against many strains of flu). There must also be intensive research on adjuvants—chemicals that enhance the immune response to vaccines. The CDC must stop demanding discounts that discourage manufacturers, and regulators should pursue agreements on “reciprocity” of approvals so that vaccines and antiviral drugs licensed in certain foreign countries can be marketed in the United States.
In the longer term, Congress could take steps to improve the climate for vaccine makers, such as offering tax breaks to offset research and development costs; requiring health insurance providers to cover immunizations without the usual deductibles; and stipulating that once the Food and Drug Administration has approved a vaccine, the government would compensate victims of known side effects.
| The best hope for coping with a pandemic is that it won’t occur within a year or two and that vaccine development will advance significantly before it strikes. |
A flu pandemic will require triage and hard-headed decisions on many levels, including not only judgments about which patients are likely to benefit from scarce commodities such as drugs, vaccines, and ventilators but also broader public policy choices about how best—among, literally, a world of possibilities—to expend resources. As has not been the case since World War II’s Manhattan Project to develop the atomic bomb, we need a robust partnership between government, universities, and the private sector to counter this universal and dire threat.
To prepare for a possible catastrophe, we need to be aggressive, innovative, and, above all, resilient. In society, as in biology, survival requires nothing less.