- Law & Policy
- Health Care
The medical liability system is in serious trouble. Injuries due to poor medical care are the leading cause of accidental death in the United States. According to the Institute of Medicine, between 44,000 and 98,000 deaths a year are caused by medical mistakes. Medication errors alone account for approximately 7,000 deaths a year, exceeding the number of deaths due to workplace injuries. And when a person is injured, the system functions more like a lottery than a rational compensation scheme. According to the Harvard Medical Practice Study, only one in fifteen patients who suffer an injury because of medical negligence receive compensation; by contrast, five out of six of the cases that receive compensation show no evidence of negligence.
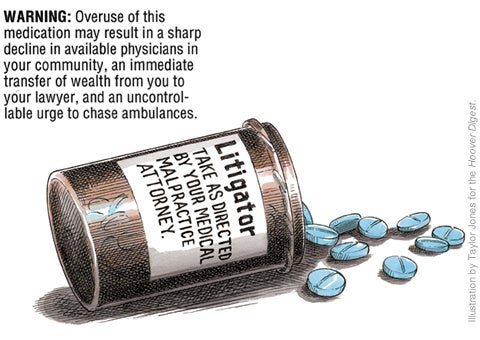
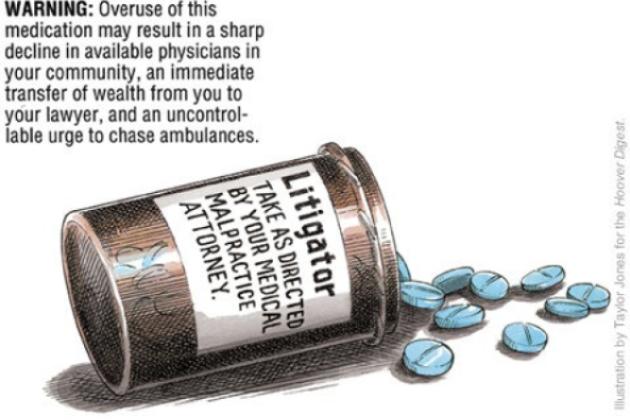
At the same time, the system is tremendously costly. Litigation expenses and other transaction costs account for more than half of malpractice compensation expenses. "Defensive medicine"—treatment decisions based on fear of legal liability rather than on patients' best interests—further drives up health-care costs and reduces access to care.
What should we do? Conventional tort reforms, such as reasonable caps on noneconomic damages, are a good first step. Caps reduce the malpractice pressure on doctors and hospitals and, in turn, reduce the prevalence and cost of defensive medicine—without significant or substantial consequences for quality. In a series of papers, Mark McClellan and I have documented how reforms reduce health-care costs. We analyzed the hospital expenditures and health outcomes of elderly Medicare beneficiaries with serious cardiac illness in the 1980s and 1990s. We found that patients from states with reforms such as caps had lower expenditures for their hospital care but the same rates of mortality and complications.
Conventional reforms have other beneficial effects. In an article in this June's Journal of the American Medical Association, David Becker, Bill Sage, and I investigate the effect of reforms on physician supply. We find that states adopting reforms such as caps on damages showed approximately 3 percent greater growth in the supply of physicians than states without reforms. An independent analysis published in Health Affairs by William Encinosa and Fred Hellinger, reaches virtually the same conclusion. This expansion in supply not only improves access but also enhances competition among physicians, which helps keep costs down and quality up.
But defensive medicine is only part of the problem. For this reason, researchers and policymakers should take up three other ideas to reform the liability system.
First, patients and their health-care providers should be given more freedom to experiment with alternatives to the courts. Second, we should reform an important rule of evidence. Data on adverse medical events collected by providers to improve the quality of care should not be admissible in malpractice cases. Third, it should be easier to use clinical practice guidelines (written statements of what constitutes appropriate treatment for a specific illness, set of symptoms, or type of patient) in malpractice trials.
Stay tuned for details next week.