- Economics
- Law & Policy
- Regulation & Property Rights
- Health Care
Suppose a group of medications were dirt cheap to produce, had virtually no side effects, and provided relief to 30 percent of those taking them. And further suppose that these benefits required no long, costly scientific studies to validate the medications’ effectiveness. Should doctors be allowed to use them?
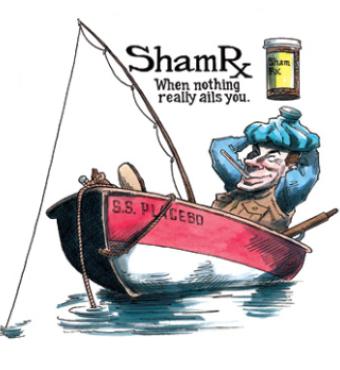
The miracle drugs I am describing are placebos—sham medicines— whose efficacy across a wide range of symptoms and conditions seems to rest on mobilizing a belief that their use will prove beneficial. Until a century ago, relatively few commonly used drugs had scientifically provable utility. Most achieved whatever benefit they provided through the placebo effect (sometimes called the “healing power of the mind”), which, while not a panacea, is by any name a surprisingly powerful force for good.
The prescriber must believe in what is being prescribed to boost the effectiveness of any medication, whether it is intrinsically “worthless” or not. Likewise, the patient must believe in what is being prescribed. The color, shape, and size of pills and capsules may influence their effectiveness. Administration by injection may convey an extra measure of potency that cannot be explained by blood levels or rates of absorption alone.
This is murky territory. Is it acceptable for physicians to deceive patients by prescribing something they know has no intrinsic merit? But where is the actual harm in harnessing a 30 percent placebo benefit, provided patients do not forgo a more effective treatment? Patients are always free to choose; when the patient’s choice is unwise, how is the physician to respond?
Medical ethicists have tended to avoid these conundrums ever since Harvard anesthesiologist Henry K. Beecher published “The Powerful Placebo” in the Journal of the American Medical Association in 1955. His opening words frame the dilemma: “Placebos have doubtless been used for centuries by wise physicians as well as by quacks.” What is one to make of that proposition?
The placebo effect touches on many common medical issues. Some analyses suggest that widely used cough medicines may help nobody at all. Why, then, have people been taking them for so long? A recent article in the New England Journal of Medicine asserts that the selective publication of antidepressant studies (the most favorable ones were most likely to be printed) exaggerated the effectiveness of some drugs, thus distorting doctors’ and patients’ expectations of their effectiveness. Another recent report, in the Journal of General Internal Medicine, indicated that almost half of Chicago physicians surveyed offer placebos to their patients—and just 4 percent let patients know they’re doing it. (Placebos in this case include not only sugar pills but also drugs that the provider doesn’t think are necessary, such as antibiotics for a viral infection.)
I recently asked two freshmen medical students what they thought of placebos. The only legitimate use they knew of was in placebo-controlled drug trials, which compare an actual medication with an identical- looking sham medication. Within my own career in internal medicine, the function of placebos was far broader. In the 1950s, when I went to medical school, their use was common. Several manufacturers sold placebo tablets to physicians and pharmacies; patients were not told that the ingredients were inert. The famed “Kings County Hospital mix” (in Brooklyn) consisted of powdered charcoal and black pepper in a bitter red liquid. It sparkled in the light and went straight to the top of your head. One teaspoon was said to cure anything, probably because nobody wanted another one. I can attest to its effectiveness in the clinics.
I fled from an offer to practice in the 1960s when I discovered that the office was full of patients getting mostly placebo shots with no doctor present. This struck me as unsafe, unnecessary, and primarily financially motivated (interestingly, such practices are found in China today).
MIND OVER MALADY
The isolation of beta-endorphin in 1975 led to the discovery that people who had been given a placebo experienced elevated endorphin levels and pain relief after wisdom teeth had been extracted. Other studies showed that headache, angina pectoris, and arthritis pain also were relieved in those who responded to placebos. A 1977 Saturday Review cover article by editor Norman Cousins, titled “The Mysterious Placebo—How Mind Helps Medicine Work,” popularized such experiences.
Later advances in neuroscience made the placebo less mysterious, allowing researchers to watch patterns of brain activity under experimental conditions. Now we know that the anticipation of a reward, whether physical, material, or emotional, lights up the same centers in the brain that are activated when the reward actually appears. The same thing happens, in a mirror image, with the anticipation and reality of pain.
Thus there is reason to believe that placebos, far from tricking or deceiving their recipients’ brains, instead predispose them to a positive response. That does not resolve the ethical dilemma of achieving an expected good end by withholding pertinent information about the means to that end, but it is far from clear how many patients would object to this. How many might say, “I want to know exactly what I am being given”; how many others would say, “As long as it’s safe, I don’t need to know—just get me better”? (Not to mention how many might say one thing and do another.)
In a 1978 article in the Archives of Internal Medicine titled “Legitimate Indications for Intramuscular Injections,” I wrote about the confusion surrounding placebos. One cited author called them “a neglected asset in the care of patients”; another considered placebos the most widely prescribed category of drugs. I wrote that “deliberate placebo use is too close to fraud, too open to abuse and too contrary to the scientific method to be acceptable.” At the same time, I pointed out that “the individual physician may (nevertheless) find himself at war within; his scientific self may reject placebos in any form, but his pragmatic self may raise nagging questions. Is there a place for the discriminating use of placebos?”
It had, by then, became unfashionable to “deceive” patients by using pseudo-medicines—whatever their benefits. Instead, physicians began to substitute very low doses of real medicines (like thyroid hormone), thinking of them as placebos but being able to claim the physiologic effectiveness usually seen at higher doses if challenged to provide a rationale for their use. The lingering legacy of this practice is found in those patients who take a quarter of a grain of animal thyroid extract daily, a dose unlikely to adequately treat any significant disease.
Even such mild subterfuges gradually came to be seen as unscientific and were replaced by prescribing “real” medicines for illnesses in which placebos might have sufficed in the past. The benevolent use of placebos to treat patients with psychosomatic symptoms as an alternative to starting with more powerful and dangerous drugs also fell victim to the new orthodoxy. Thus the solution to the old problem created a new one: real medicines all have real side effects. There is now no legitimate way to prescribe placebos while fully informing patients and providing so-called evidence-based care that depends solely on proven therapies. Significantly, this is the standard that governs reimbursement by Medicare and private insurance carriers.
Where do leading medical organizations stand on the ethics of placebos? The American Medical Association seems opposed to their use. The second of seven of its Principles of Medical Ethics condemns fraud or deception. Placebos are consequently allowed in clinical trials and possibly in practice, but only with informed consent. Few physicians seem likely to prescribe them if they first have to explain what they are. Imagine how embarrassing it would be to admit that anything else might work equally well.
The Charter on Medical Professionalism, created by a consortium of American and European medical organizations in 2002, states in a comment on patient autonomy: “Physicians must be honest with their patients and empower them to make informed decisions about their treatment.” The use of sham medicines without informed consent is clearly not authorized. Likewise, the 2005 Ethics Manual of the American College of Physicians speaks only about using placebos in clinical trials, and even then finds their use “only occasionally acceptable” if a proven alternative to the new drug being studied is already available for comparison.
In contrast, the Chicago study, which was done by surveying practicing doctors with academic appointments, confirms that placebo use is still widespread. There must therefore be a significant degree of silent public complicity; drug information is too widely available today for placebo administration to succeed without willing partners.
My approach, in cases where worry seems more prominent than illness, is to issue a prescription for an appropriate medication (typically for complaints such as erectile dysfunction or mild depression) and advise the patient not to fill it for a week. If the problem persists, the prescription is to be filled but not taken for another week. Only if there is still no improvement will actual drug treatment begin. I see this as both honest and effective. Understanding, reassurance, and the expectation of continued care often resolve the problem without needing to use drugs.
A PUZZLING LACK OF APPRECIATION
Physicians who concentrate on perfecting the science of what they do are often puzzled that patients fail to be more satisfied with their efforts. American health consumers actually go more often to practitioners of alternative medicine, whose therapies may delay more effective science-based treatments, than they do to U.S. primary-care physicians. Why are patients, voting with their feet, seeking out alternatives that maximize the placebo effect even as evidence-based medicine—the new “prove it or lose it” standard for medical practice—tries to eliminate it?
My answer is that the zealous application of pure science to patient care can be too abstract and mathematical. Individual differences tend to get lost in the mathematics. A drug that beats out another medication in a study by 55 percent to 45 percent may win election to the approved-drug list of an HMO, but there may still be people among the 45 percent for whom the less-effective drug works better. On the other hand, a drug may be even more effective than its performance in a classic double-blind, placebo-controlled trial indicates—precisely because the potentially useful placebo effect has been deliberately taken out of consideration.
Until we have a far better understanding of individual differences, pure science cannot be used to arbitrarily make policy, let alone as a guidebook for human behavior. If it could, fewer people would gravitate toward alternative medicine and fewer physicians would be looking for imaginative ways to responsibly use placebos.
Alternative practitioners should not be the only ones allowed to tap the imperfect yet often potent power of placebos. We can devise safeguards to ensure responsible use and pass laws to resolve ethical and insurance coverage issues. As for medical science, it can still flourish without contemptuously rejecting the less than perfect when it has not yet found better alternatives.
Stanford medical ethicist Margaret Eaton disagrees. She says, “As neuroscience learns more about the mind-body connection, physicians will learn to harness and promote the body’s ability to heal without toxic drugs and without resorting to the deception required to prescribe placebos.”
Perhaps so. But when? At what cost? And what about now?