Click here to download this proposal.
Supply-side solutions should be aimed at increasing healthcare choices. That will require reducing federal and state regulatory burdens. To that end, the Choices for All Project proposes key incremental improvements that remove these barriers. We divide these reforms into two categories: reforms to regulations affecting the supply of healthcare providers and reforms affecting the types of health coverage available to Americans. In both cases, we identify reforms that could be championed by policymakers at the federal or state levels.
Key Plan Elements
More Healthcare Providers and Facilities
- Standardize and expand on Covid-era telemedicine reforms.
- Expand Scope of Practice for Nurse Practitioners (NPs).
- Expand the recognition of medical licenses across states.
- Increase reciprocity of medical licenses for foreign-trained physicians to address the shortage of primary care physicians.
- Repeal Certificate of Need laws to increase the supply of hospitals and specialized outpatient facilities.
- Reverse ACA restrictions that prevent new physician-owned healthcare facilities.
More Personalized Health Coverage Options
- Allow payments to Direct Primary Care providers to count as qualified medical expenses.
- Expand access to Association Health Plans.
- Allow Copper plans to be sold on state exchanges.
Details
Government rules and regulations affect the cost of healthcare by influencing the prices that providers can charge, the payments they receive, and the overall cost of delivering care. They also artificially restrict the supply of healthcare and health insurance options available to consumers.
Today, we are told what types of health plans we can buy, what health services must be covered, which providers we may see, and which facilities we can access. The regulations may have originally been intended to protect patients, but many have devolved into mere barriers to entry or to a more competitive healthcare landscape. They now serve an anticompetitive purpose: protecting existing players in the healthcare economy, rather than improving patients’ health.
Rather than this one-size-fits-all approach, we need a regulatory system that embraces consensus without uniformity. Artificial restrictions on the provision of healthcare can lead to predictable outcomes: higher costs, less access, lower quality, and fewer choices. Progress toward our goals of lower costs, improved access, and better-quality medical care will come from removing restrictions so that patients have more choices in how they receive care.
We divide these reforms into two categories: reforms to regulations affecting the supply of healthcare providers and reforms affecting the types of health coverage available to Americans. In both cases, we identify reforms that could be championed by policymakers at the federal or state levels.
More Healthcare Providers and Facilities
Permanently expand telemedicine authority
During the pandemic, all 50 states and Washington D.C. enacted waivers allowing telehealth services across state lines. Many of these waivers, however, were temporary; by December 2022, the waivers had expired in 39 states and in Washington D.C. While a handful of states have permanently changed their rules allowing out-of-state providers to provide telehealth services and the federal government extended many of its telehealth waivers, we propose that the federal and state waivers should be made permanent to allow healthcare providers to provide services—at lower costs—to the patients who need them. States can do this by passing streamlined registration processes for out-of-state practitioners mirroring state legislation passed in Florida in 2019 and Arizona in 2021.
Eliminate scope-of-practice rules
Currently, 23 states still restrict or reduce the “scope of practice” allowed to be performed by nurse practitioners (NPs), Advanced Registered Nurse Practitioners (ARNPs), and physicians’ assistants (PAs). Given the shortage of primary care providers in the United States, restricting the allowable level of care that NPs, ARNPs, or PAs are allowed to provide to lower than their level of training is unwise. These scope-of-practice rules limit the available supply of healthcare workers and lead to longer wait times for non-emergency services.
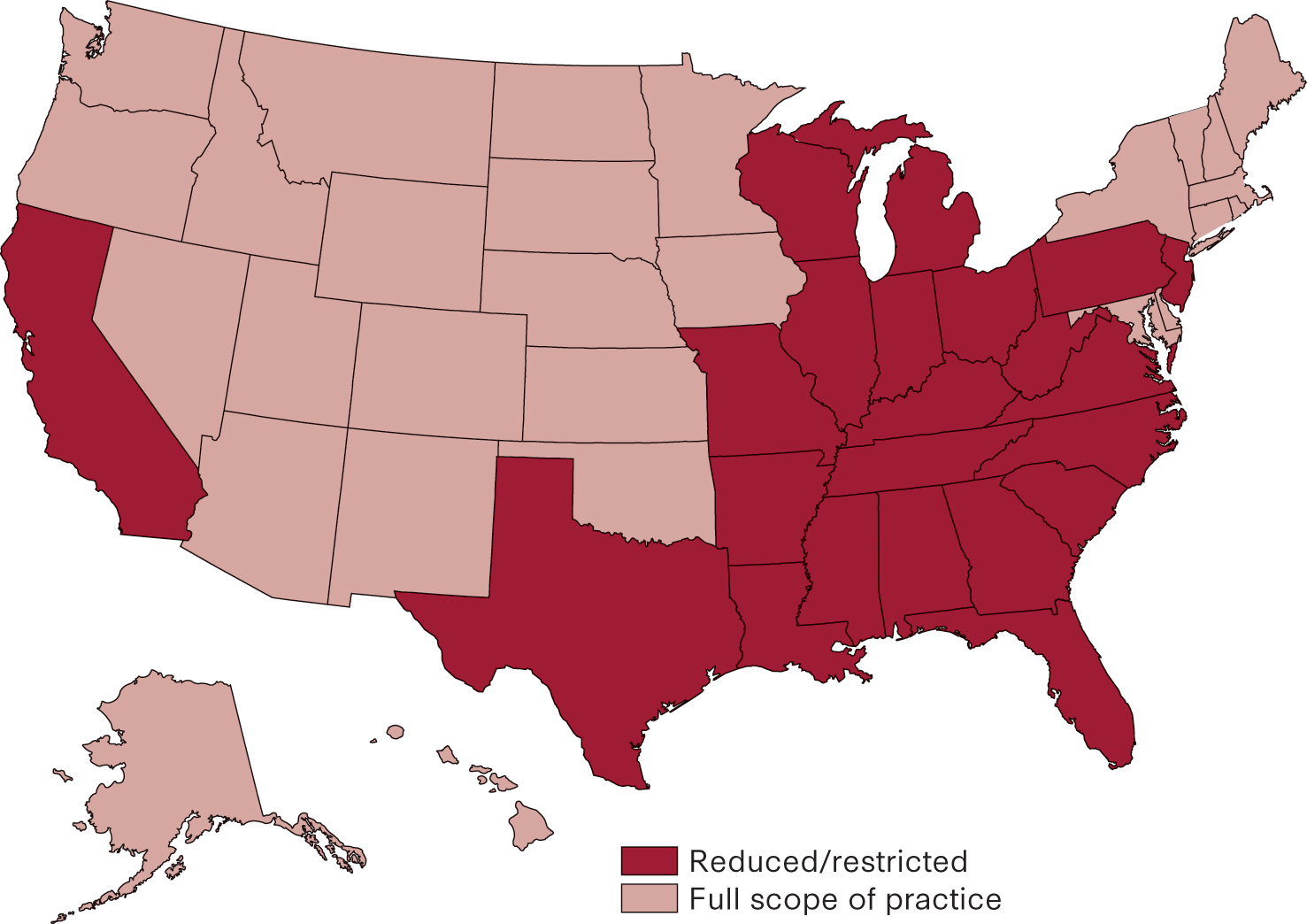
While defenders of scope-of-practice rules point to concerns over safety and the quality of care provided to the patient, multiple studies conclude that there is no association between restrictions on the scope of practice and an increase in the quality of primary care provided. Moreover, studies have found that states with full-practice authority for NPs have a larger supply of NPs, and patients, therefore, benefit from shorter wait times, more access to primary care, and fewer emergency room visits.
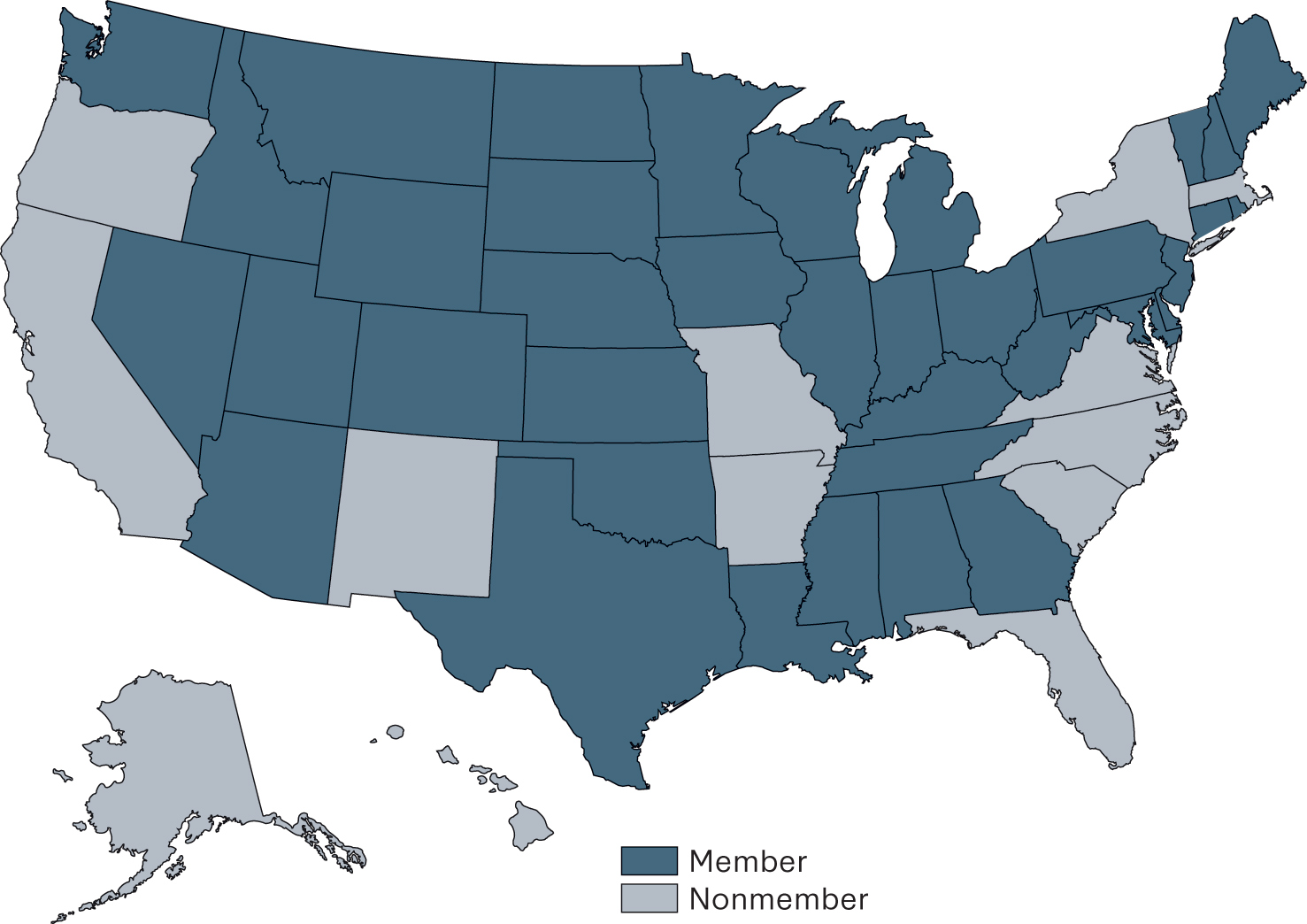
Expand recognition of medical licensing across states
The recognition of medical licenses across state lines promotes competition and expands the pool of available healthcare professionals, particularly in underserved areas. It also reduces administrative burdens and costs for healthcare professionals who practice in multiple states, allowing them to focus more on patient care. The Interstate Medical Licensure Compact and the Nurse License Compact allow physicians and nurses, respectively, to apply for a license in one state and have it recognized in other participating states. States who have yet to enter these compacts—including large ones like California, Florida, and New York, should particularly consider joining.
Reduce Barriers for Foreign-trained Medical License Holders
America is not training and producing enough physicians. In addition to ending scope-of-practice rules on NPs and other practitioners, the shortage can be further narrowed by relying on foreign-trained doctors and other practitioners. Unfortunately, it is difficult and costly for foreign-trained physicians or nurse practitioners to move to the United States and help fill this gap.
Lawmakers should embrace the reciprocity of medical licenses, in conjunction with other requirements, to encourage foreign medical professionals in good standing to practice in the United States. The recognition of foreign medical licenses could be combined with a push to increase placements in rural or underserved areas. For example, the Minnesota Department of Health has experimented with new pathways for foreign medical school graduates to practice in the state. Enacted in 2015, Minnesota’s International Medical Graduates (IMG) Assistance Program was intended “to increase access to primary care in rural and underserved areas of the state.” Among other policies, the program relaxes residency program recency requirements for international medical graduates.
Eliminate Certificate of Need Laws
Certificate of Need (CON) laws are state-level regulations requiring healthcare providers to obtain approval from a governing body before expanding, building new facilities, or offering certain services, based on demonstrated community need and financial viability. They gained popularity as a cost-saving measure when Medicare began and medical spending was rising rapidly. Over time, CON laws have been used primarily by existing medical providers to prevent new competition. By 1987, Congress repealed the federal mandates for CON laws. Despite the decades-old repeal, as of May 2020, 35 states and the District of Columbia still had some form of rules that stifle the supply of medical facilities and specialized care that could otherwise be offered to patients.
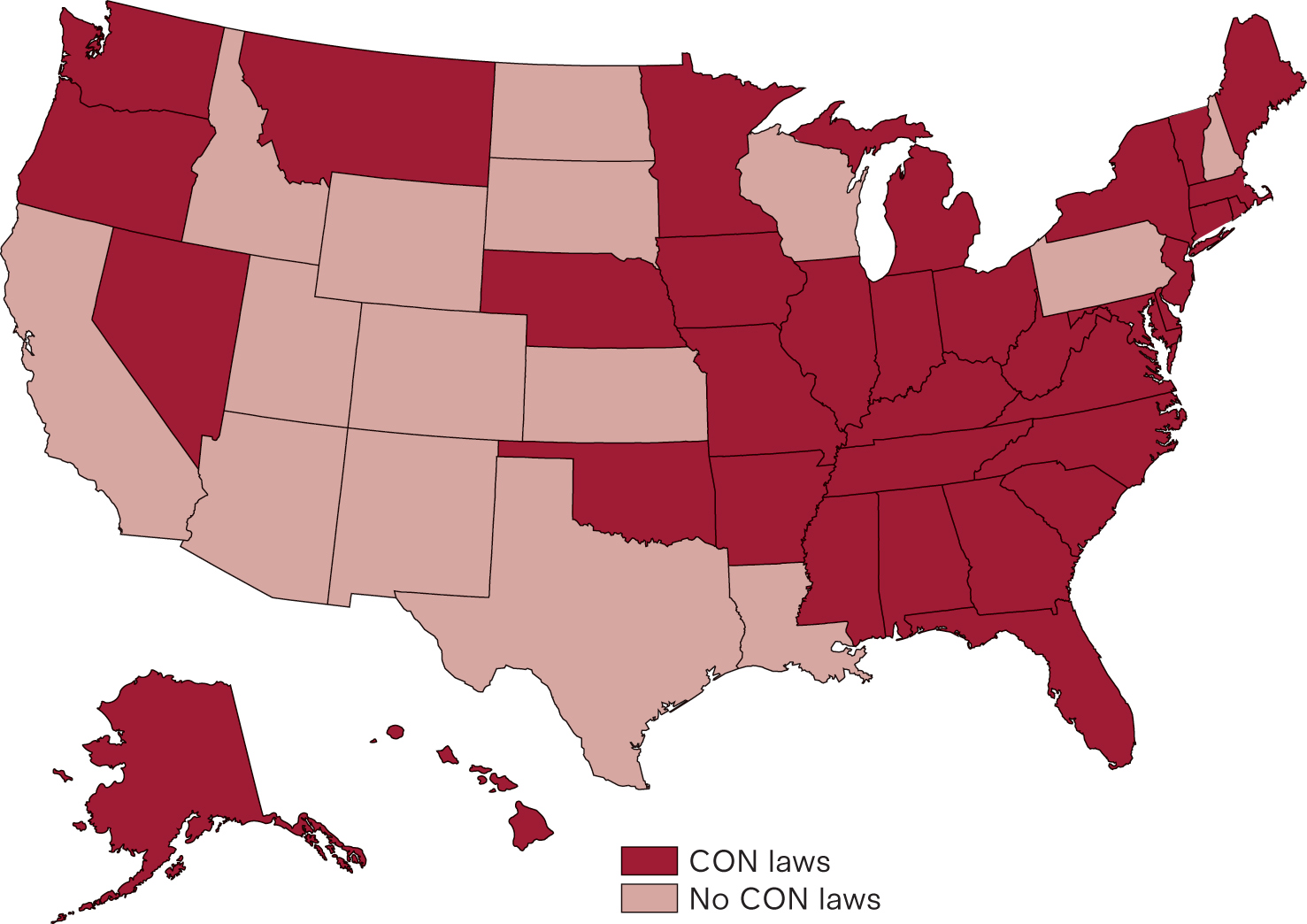
A closely related issue to CON laws is the increased use of Certificates of Public Advantage (COPA laws) by states. These laws shield hospital mergers from certain federal antitrust rules. Under COPA laws, states allow hospitals to merge but in exchange exercise increased regulatory oversight of their post-merger prices and policies. In evaluating COPA laws, the FTC has found that commercial inpatient prices rise after the introduction of COPAs.
Remove Limits on Physician-Owned Hospitals
Physician-owned hospitals (POH) are healthcare facilities such as hospitals, clinics, and surgery centers that are owned, in part or whole, by physicians. In the United States, physician-owned medical facilities have been a source of controversy due to concerns that they may lead to self-dealing that would result in higher healthcare costs and unnecessary procedures. In 2010, the Affordable Care Act (ACA) included provisions (Section 6001) that placed restrictions on physician-owned hospitals (POH). Since then, the result has been to limit competition by freezing the size of existing POHs and preventing the creation of new medical facilities.
New POHs can be built with waivers from the U.S. Secretary of Health and Human Services, but it is a political hurdle that is difficult to clear. Policymakers should instead reevaluate Section 6001’s ban on physician-owned hospitals to increase choice and produce competition among healthcare providers, particularly in rural and other areas where healthcare facilities are limited.
Personalizing Health Coverage
- Encourage Direct Primary Care
Direct Primary Care (DPC) is a new and growing method of providing primary care to patients at potentially a much lower cost, with increased access and higher levels of satisfaction for both patients and physicians. Akin to “affordable concierge care,” DPC patients pay a monthly fee (averaging around $80 a month) for expanded access to their personal physician. The monthly fee covers routine screenings, preventive care, chronic care services, and care coordination. Prescription drugs are often included at cost and DPC doctors regularly arrange discounted access to lab tests and imaging services.
Expanding the recognition of DPC membership fees as qualified medical expenses for all taxpayers would help to increase the number of DPC practices available nationwide and help shift predictable and routine care to a more cost-efficient setting. Improving access to DPCs isn’t just for those with employer coverage; in our chapter on Medicaid and ACA reforms we highlight how expanding access to DPC can be particularly useful for low-income Americans who currently face long waits and poor outcomes in their state Medicaid programs.
- Expand Access to Association Health Plans
Association Health Plans (AHPs) are group health insurance arrangements allowing businesses, especially small and mid-sized enterprises, and self-employed individuals, to band together and purchase health coverage collectively. By pooling resources and spreading risk, AHPs aim to provide more affordable and accessible insurance options for enrollees. They also allow small businesses the ability to negotiate like a larger employer with insurers on cost and obtain medical claims data too, if the AHP is self-funded.
However, AHPs are limited by numerous rules and regulations. The Employee Retirement Income Security Act (ERISA) strictly limits the definition of an employer or association, making it difficult for multiple businesses to form AHPs. State insurance regulations prevent AHPs from forming across state lines or offering consistent coverage for mobile employees. Federally, the ACA’s requirement of minimum essential health benefits limits possible AHP plan designs and raises costs. In the past, lawmakers have tried to expand the use of Association Health Plans but were unsuccessful in passing their reforms.
Expressly permitting Association Health Plans to be formed by self-employed individuals or small businesses in similar industries would lower their costs while giving them more options for insurance coverage. Congress should go further by exercising its right to regulate interstate commerce and expressly allowing AHPs to form across state lines. In conjunction with expanded OOP deductibility or Individual Health Accounts (see our chapters on reforming the tax code for more details), more families and individuals would be able to get coverage that better matches their needs.